Advanced practice providers (APPs), like nurse practitioners (NPs) and physician assistants (PAs), are responsible for diagnosing a wide range of illnesses and injuries, developing treatment plans and educating patients on how to prevent chronic disease. Due to increased demand for healthcare services, insurance industry changes and a shortage of physicians, the U.S. Bureau of Labor Statistics (BLS) predicts employment of NPs and PAs will grow much faster than average between 2021 and 2031.
The BLS expects the job outlook for nurse practitioners to increase by 46% from 2021 to 2031. It also projects that the number of physician assistant jobs to increase by approximately 28% during the same period.
Since APPs are in such high demand, it’s essential to understand the differences between NP and PA careers. This guide provides an overview of both roles, with information on transitioning from your current healthcare role to an advanced practice career.
Growth of NP and PA Roles
“What is an advanced practice provider?” is a common question people interested in advanced healthcare careers may ask. APPs are health professionals who perform many of the same activities as physicians, even though they haven’t attended medical school. Nurse practitioners and physician assistants are advanced practice providers with more training than nurses and medical assistants but less training than doctors, making them mid-level providers. Due to the changing healthcare landscape, NP and PA roles have evolved, allowing them to perform more advanced tasks.
Nurse Practitioners
In the 1960s, two doctors from Colorado created the NP role to make it easier for underserved populations to access healthcare services. While nurse practitioners have always provided high-quality care, the NP role has evolved to meet the changing needs of patients, healthcare facilities and health insurance providers.
Shortly after the introduction of the NP role, Congress passed the Social Security Amendments of 1965, creating the Medicaid and Medicare programs. Both programs increased access to healthcare, but some regions didn’t have enough physicians to handle the influx of patients. NPs played a vital part in providing primary care to these populations.
Since then, NPs have expanded their scope of practice, allowing them to use their skills in a much more comprehensive range of specialties. Common specialty areas include family practice, women’s health, psychiatric/mental health, pediatrics, neonatal health and adult-gerontology care.
According to the American Association of Nurse Practitioners (AANP), more than 355,000 NPs are licensed to work in the United States. Due to the increased demand for care, many states have also given nurse practitioners full practice authority (FPA). In these states, NPs evaluate patients, make diagnoses, develop treatment plans, interpret diagnostic tests and prescribe medications under the authority of the State Board of Nursing.
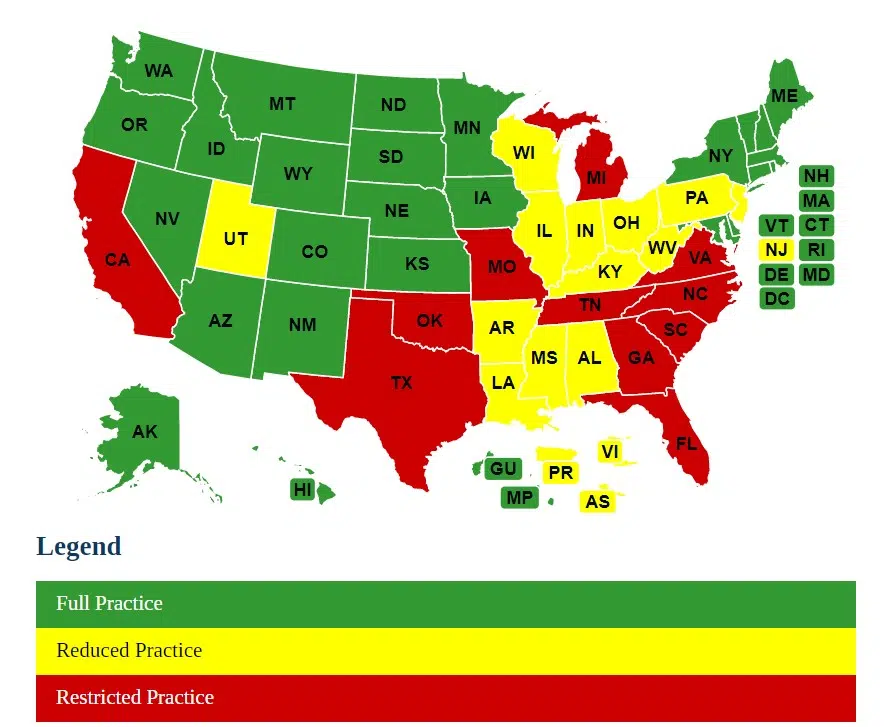
The AANP also reports that NPs have FPA in 26 states, the District of Columbia, Guam and the Northern Mariana Islands as of October 2022. Only 11 states restrict NPs’ ability in one or more practice elements and require career-long supervision, delegation or management by another health provider regarding patient care. The remaining states and U.S. territories reduce NPs’ ability in one or more practice areas and require a career-long collaborative agreement with another healthcare provider.
Source: AANP
Physician Assistants
The first physician assistants graduated from Duke University’s PA program in 1967. Dr. Eugene Stead started the program to help address a shortage of primary care physicians, which made it difficult for some patients to receive high-quality care. Less than a decade later, the National Board of Medical Examiners started offering national PA certification exams.
However, it wasn’t until 2016 that all 50 states and the District of Columbia decided to adopt licensure as the standard regulatory term used to describe a PA’s status. Previously, some states referred to PAs as certified or registered, causing confusion for patients and their family members. Every location now uses the term licensed to describe a PA’s credential. The Kaiser Family Foundation listed 119,789 physician assistants as licensed to work in the United States in August 2022.
According to the American Medical Association (AMA), all 50 states require PAs to have some form of a supervisory or collaborative arrangement with a physician. However, the exact requirements within these agreements vary. Many states require physician assistants to be supervised by physicians, which may involve cosigning orders or taking other supervisory actions.
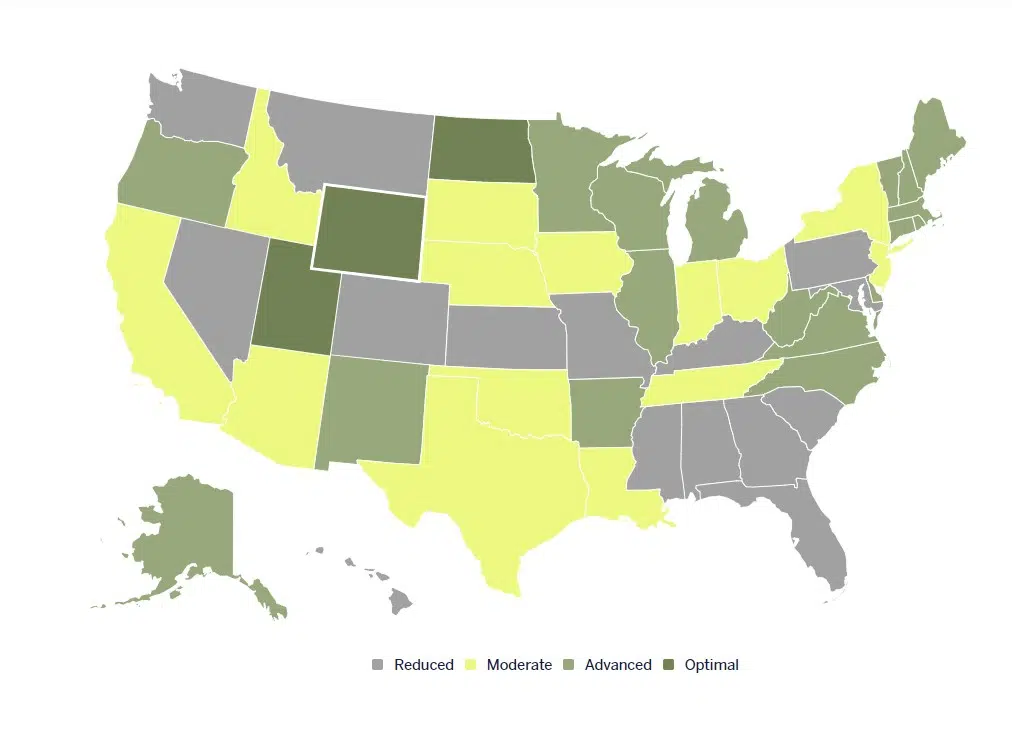
The American Academy of Physician Associates (AAPA) lists four distinct categories of practice authority for PAs, including Optimal, Advanced, Moderate and Reduced. Only a few states have adopted Optimal guidelines allowing PAs to practice to the full extent of their education, training and experience while still requiring collaborative agreements.
Source: AAPA
Drivers of Demand for NPs and PAs
One of the primary reasons APP roles have grown over the past decade is the United States has fewer physicians than are needed to meet the growing demand for healthcare services. The Association of American Medical Colleges expects a shortage of 37,800 to 124,000 physicians by 2034. People are also living longer, which means many may develop more serious illnesses. Medical facilities need trained NPs and PAs to help care for the aging patient population.
Furthermore, some insurance companies have reduced reimbursement rates, forcing medical facilities to do more with less. One way to manage costs is to hire fewer physicians and more APPs to ensure patients have continued access to high-quality care. Due to proposed changes in Medicare reimbursement rates, the potential of pandemics affecting millions of people and other trends in the healthcare industry, the NP and PA roles may evolve even more over the next decade.
Common APP Job Duties
Nurse Practitioners
NPs provide primary care, specialty health services and treatment for acute illnesses and injuries. Although the duties of an NP vary slightly based on their practice setting, all nurse practitioners receive training in the following:
- Ordering and interpreting blood and urine tests
- Conducting physical examinations
- Prescribing medications
- Developing patient treatment plans
- Ordering and interpreting imaging studies
- Recommending appropriate screening procedures
- Counseling patients on healthy lifestyle choices
- Managing chronic health conditions
- Treating respiratory infections, urinary tract infections and other acute illnesses
Specific duties may vary based on the NP’s patient population focus. For example, psychiatric/mental health nurse practitioners (PMHNPs) focus on patients with psychiatric or mental health needs. PMHNP duties may involve conducting mental health assessments, diagnosing mental health conditions and determining a plan of care. They may also work with family members to identify socioeconomic risk factors for mental illness.
To become a certified nurse practitioner, you must have an NP-focused Master of Science in Nursing (MSN) or doctoral degree from an accredited college or university. You must also pass a national board certification exam based on patient population, such as:
- Adult-Gerontology
- Women’s Health
- Family Practice
- Pediatrics
- Neonatal Health
- Oncology
- Orthopedics
- Psychiatric Health
Physician Assistants
In collaboration with physicians, PAs are responsible for evaluating patients, diagnosing their illnesses and injuries, developing treatment plans and following up as needed. PAs may also perform the following duties:
- Ordering lab tests and X-rays
- Performing physical examinations
- Administering immunizations
- Educating patients on disease prevention
- Promoting healthy habits
- Reviewing patient medical histories
- Stitching wounds
- Setting broken bones
Duties may vary based on the practice setting. For example, women’s health PAs may routinely perform pelvic exams, while a urology PA may spend more time working with male patients with prostatitis, benign prostatic hypertrophy and other urological conditions.
To become a physician assistant, you must complete a bachelor’s degree and work a minimum number of hours in a job involving direct patient care. You must also pass several rigorous science courses. Once you satisfy these requirements, you must complete a PA education program accredited by the Accreditation Review Commission on Education for the Physician Assistant (ARC-PA). To become Physician Assistant-Certified, you must pass the Physician Assistant National Certifying Examination.
Best-Paying NP Specialties
As a job market resource, Vivian Health collects salary data for various healthcare professions. Based on our data, nurse practitioners are among the highest-paid advanced practice RNs. Among NP specialties, some of the highest-paid NPs during the first week of December 2022 included:
| NP Specialty | Average Hourly Rate |
| Neonatology | $59 |
| Family Nurse Practitioner | $65 |
| Pediatrics | $72 |
| Psychiatric Nurse Practitioner | $90 |
Best-Paying PA Specialties
According to the AAPA, the highest-paying PA specialty is cardiology and cardiothoracic surgery, which pays an average of $147,200 per year. Emergency medicine and surgical subspecialties round out the top three highest-paying PA specialties, with average salaries of $129,146 and $127,775 annually, respectively.
Travel Opportunities for Advanced Practice Providers
During the COVID-19 pandemic, travel roles for nurse practitioners increased dramatically. As a result, Vivian regularly posts travel opportunities for NPs interested in pediatrics, critical care, psychiatry, cardiothoracic surgery and family practice, among others.
Physician assistants have similar prospects, with travel opportunities for physician assistants wanting to provide specialty care, especially in cardiothoracic surgery, critical care, neurosurgery and oncology. Many facilities also need travel PAs for family practice and pediatrics.
Due to the increased demand for advanced practice providers, NPs and PAs have tremendous negotiating power. You may be able to negotiate a higher-than-advertised salary based on your experience or some type of bonus.
Overall Salary Potential and Demand for APPs
Based on Vivan’s salary data from December 5, 2022, from employers around the nation, staff nurse practitioners earn an average hourly salary of $65, with some positions paying up to $90. Staff physician assistants earn an average hourly rate of $74, with some positions paying up to $87. You may earn more depending on your location, experience level and willingness to take on travel jobs.
Whether you want to become a nurse practitioner or a PA, the outlook for both careers is strong. With these roles in high demand, transitioning from your current healthcare role to an advanced practice career is a wise decision and an investment in your future.